Introduction
Sickle cell disease (SCD) is an hereditary hemoglobin disorder characterized by repeated episodes of severe acute pain, acute chest syndrome (ACS) and other complications. The average life expectancy of SCD patients remains 20 years less than the general population, and ACS is the leading cause of mortality. This retrospective study describes the effect of the COVID-19 pandemic on epidemiologic trends and outcomes of Acute Chest Syndrome.
Methods
The National Inpatient Sample (NIS) database from 2016 to 2020 was searched for hospitalizations with ACS as the principal diagnosis using Clinical Classifications Software Refined codes. The ACS admission rate for each calendar year was obtained as admission per 10,000 SCD adults hospitalized. The primary outcome was a comparison of inpatient mortality, and the secondary outcomes were the length of hospital stay (LOS) and total hospital charge (THC) between prepandemic (2019) and pandemic years (2020).
Results
In 2019 (prepandemic), there were 5,160 hospitalizations for ACS, accounting for 624 per 10,000 adult SCD hospitalizations. In 2020 (pandemic), there were 4,285 patients hospitalized for ACS, accounting for 540 per 10,000 adult SCD hospitalizations. The mean age of admission was similar for both years (31.5 vs 32 years, P=0.143), and there was no significant difference in age categories when both years were compared. The gender distribution was similar during both periods (females: 45.6 vs 46.7%, p=0.68). The racial distribution was predominantly blacks with no significant difference during both year (92 vs 92%, p=0.3). There was no significant difference in hospitalizations with regard to insurance status, hospital region, or hospital size between both years.
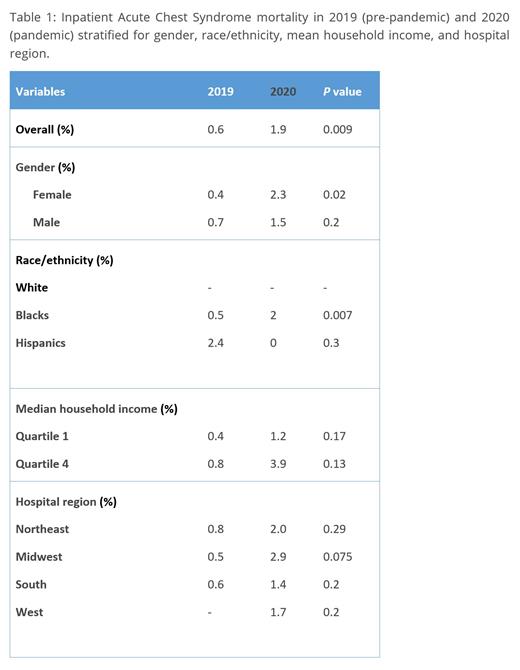
There was a three-fold increase in overall proportion of ACS inpatient mortality in the pandemic year of 2020 compared to the prepandemic level (0.6% vs 1.9%, P=0.009). Proportion of mortality among women had a five-fold increase (0.4% vs 2.3%, P=0.02). There was a four-fold increase in mortality proportions among the Black population (0.5% vs 2%; p=0.007). Mortality outcomes were similar over both years when stratified for income quartiles and hospital regions.
The LOS during the pandemic was similar to the prepandemic level (6.5. vs 7.4days, P=0.563). Also, there was no statistically significant difference in the total hospital charge ($61,515 vs $80,191, P=0.108).
Conclusion
This study depicts a statistically significant increase in inpatient mortality outcomes of Acute chest syndrome during the pandemic period. However, the length of hospital stay and total hospital charge were similar. Further studies need be conducted to evaluate the long-term effect of the COVID-19 pandemic on SCD.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal